Untangling the Message: Strategy and Systems Thinking Improve Communication for Veterans
Client: Veteran Affairs
Timeline: October 2022 - July 2025
Role: UX researcher, design strategist, and primary stakeholder POC
From Insight to Execution:
1. Tackled a naming problem with real-world consequences
Veterans were confused by provider contact names filled with unclear acronyms and inconsistent formatting.
2. Mapped the impact on care and trust
Messages were misrouted or delayed. Veterans gave up on contacting providers, and coordinators were burdened with rerouting tasks.
3. Ideated a low-lift, high-impact solution
Leveraged existing APIs and health taxonomy work to offer Veterans familiar identifiers like provider name, facility, and care type.
4. Faced delays despite validation
Even with prototype-ready solutions and multiple rounds of confirming research, lack of stakeholder support stalled implementation.
5. Strategy realized, years later
Two years after the original research, the proposed solution was finally implemented, validating the strategy and providing long-term impact.
Background: Modernizing Secure Messaging for VA.gov
As part of the Digital Health Modernization strategy, the Department of Veterans Affairs is consolidating key health tools into a single, streamlined experience on VA.gov. One of the most critical tools being migrated is Secure Messaging, which allows Veterans to send non-urgent messages to their care teams.
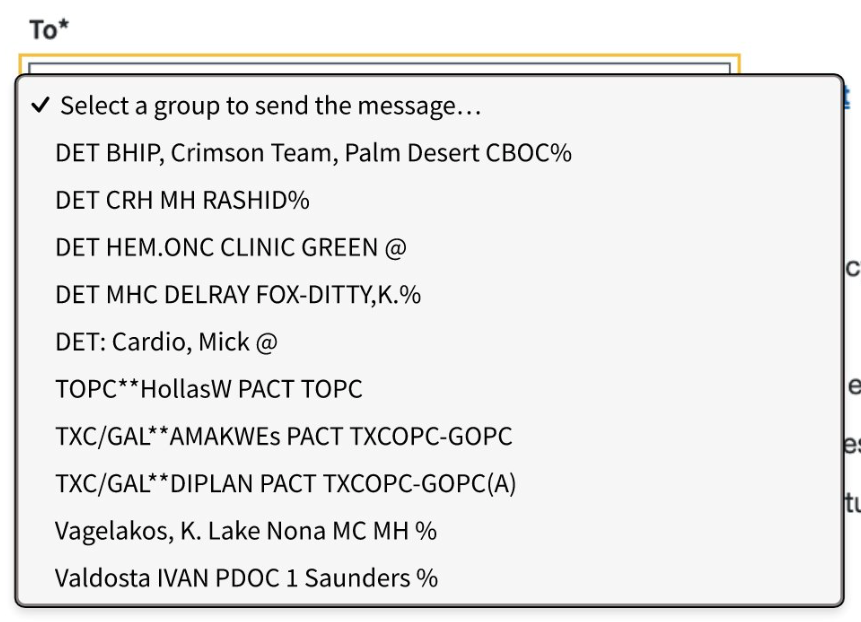
However, confusing naming conventions, including acronyms, abbreviations, and symbols, make it difficult for Veterans to identify the right provider or care team.
The example shown here reflects the current experience, where message recipients are listed with inconsistent and often indecipherable formatting.
Discovery Highlighted a Barrier to Veteran Care
To understand the impact of provider contact (triage group) naming on Veterans’ experience, I triangulated data collected from interviews and surveys with My HealtheVet coordinators, health taxonomy experts, and system administrators, alongside insights gathered from Veterans during usability testing.
What we found was clear:
11% of provider contact names did not follow national conventions.
81% of the inconsistencies were concentrated in just 17 facilities.
Veterans struggled to understand the naming patterns due to acronyms, symbols, and inconsistent formatting.
These naming issues had real consequences:
Messages were misrouted or delayed, disrupting care.
Veterans lost trust in the system.
Some abandoned the task entirely, giving up on messaging their provider.
Coordinators were forced to spend time manually rerouting messages, creating additional administrative burden.
The findings pointed to a breakdown in communication that impacted both care delivery and trust, highlighting the need for clear, Veteran-centered naming and labeling.
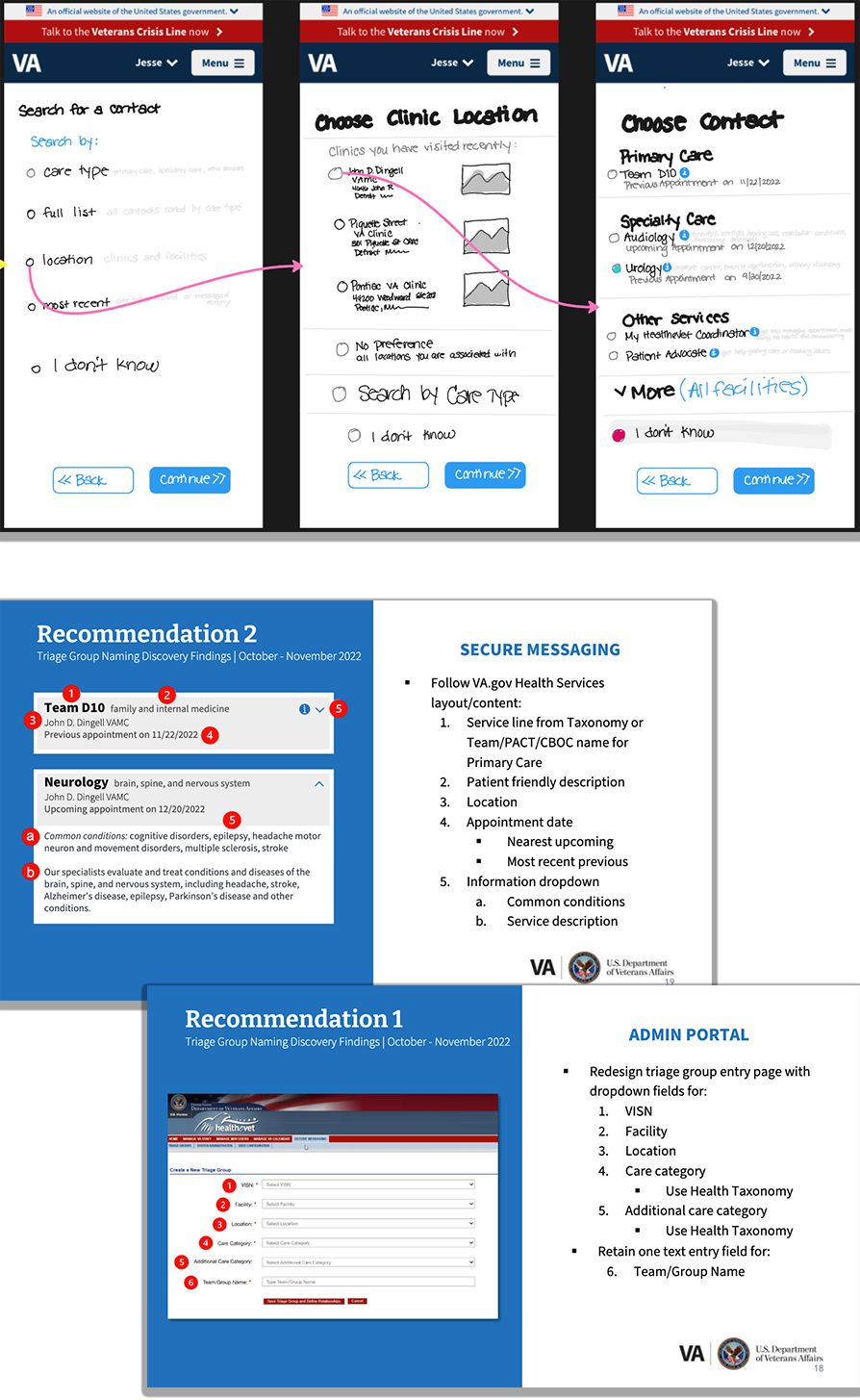
Strategic Ideation: Using Existing Infrastructure to Improve Clarity
To address the breakdown in naming consistency and improve clarity for Veterans, I strategized a solution that leveraged existing infrastructure, minimizing disruption while maximizing usability.
My approach combined:
The VA Health Taxonomy to anchor contact names in recognizable care categories
The Facilities API and Appointments API to surface relevant provider data
A stepped flow that helped Veterans locate the right contact by:
Type of care
Facility or location
Most recent interaction
To implement this solution, only minimal changes were needed in the admin portal used by MHV coordinators - specifically, the addition of care category and location fields when entering contact names.
This approach respected both technical constraints and user needs, creating clarity without adding burden.
Progress Paused: Navigating Stakeholder Hesitation
Even though we had fully developed prototypes ready for testing, stakeholders ultimately declined to move forward with usability validation, stalling momentum on a solution that directly addressed known pain points.
In August 2023, they approved a limited round of generative research, which confirmed that Veterans rely on:
Location
Type of care
Appointment history
as primary identifiers when selecting a message recipient.
Despite this validation, no further progress occurred for nearly a year.
Final design by Joel Calumpong
We had the right data, the right design, and the right moment, but not yet the green light.
Validation Built on Earlier Work
In July 2024, stakeholders conducted an unmoderated study to explore solutions for improving provider contact clarity in Secure Messaging. The two concepts they tested both incorporated the key identifiers I had previously researched and proposed:
Location
Type of care
Provider name
Although I was no longer actively engaged in the project, the study relied heavily on the discovery research and strategic ideation I led in 2023.
The product lead acknowledged and thanked me for the foundational work, recognizing that the direction and structure had been shaped by my earlier contributions.
The study reinforced what we already knew: Veterans identify their care teams by who they see, where they go, and what type of care they receive.
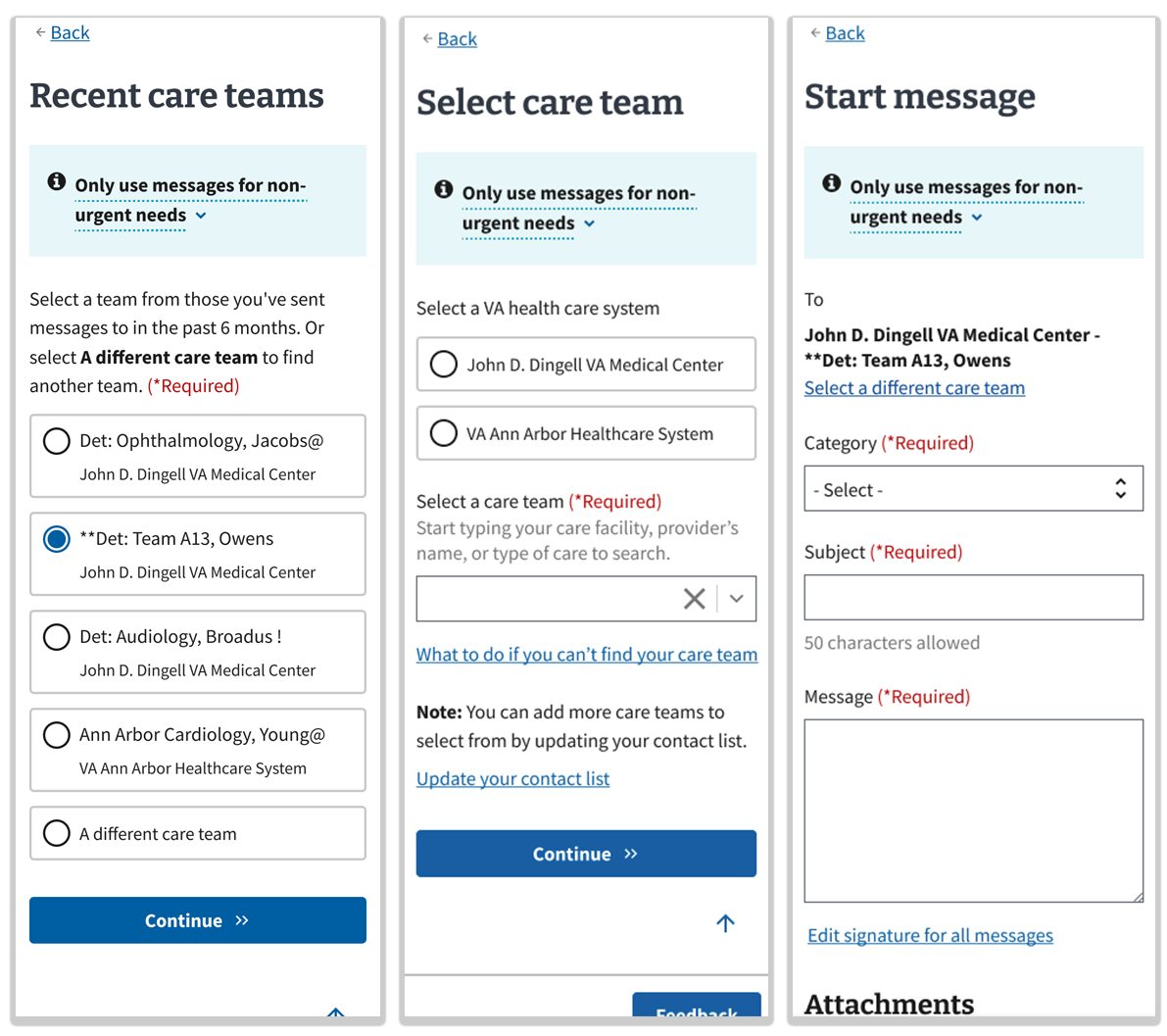
Long-Term Strategy, Finally Realized
In spring 2025, the upcoming integration of My VA Health data into My HealtheVet (driven by the migration from VistA to Oracle Health) reignited focus on improving Secure Messaging.
The solution concepts I proposed two years earlier were finally designed and implemented:
Veterans now see their recent care teams first, streamlining selection.
Facility location is prominently used as a key identifier.
Acronyms and symbols are being addressed separately, with a pilot planned for summer 2025.
Final design by Emily Taylor and Ben Caldwell
While the rollout was delayed, these changes reflect the strength of research-driven strategy, and how the right solution can still surface, even after years of organizational inertia.
Strategy Validated by Usability Testing
My team conducted remote moderated usability testing with 9 Veterans to evaluate whether the new design helped them find and message the right care team. Tasks focused on selecting recent providers, searching for care teams, and using fallback options when contacts weren’t found.
All 8 participants who were tasked with sending a message to a recent provider found and selected the correct provider on the recent recipients list.
All 9 participants successfully located and messaged two providers by first identifying the location.
This showed the broader search flow was intuitive.
The solution proved intuitive and effective, empowering Veterans to find the right contact quickly. This validated the strategy of using recent care teams, provider names, and facility details as primary identifiers.
Strategy That Withstood the Test of Time
This work wasn’t a sprint, it was a strategic marathon.
Over two years, I navigated shifting stakeholder priorities, legacy system constraints, and institutional hesitation to advocate for a solution grounded in Veteran needs.
I connected insights from multiple research efforts and data sources
I made the case for long-term strategy over short-term fixes
I ensured Veteran experience remained central, even when the project stalled
These designs were in development as my team’s contract ended in July 2025 and are expected to be deployed by the end of summer.
This journey shows how thoughtful strategy, rooted in research, can outlast delays, influence decisions, and ultimately shape systems that serve Veterans better.